Getting your Trinity Audio player ready...
For years, the prevailing assumption has been that pelvic pain during pregnancy resolves after childbirth. However, many women continue to experience such pain months – or even longer – after delivery. Research indicates that about two-thirds of pregnant women suffer from pelvic and lower back pain during pregnancy, with some developing chronic pain that significantly disrupts their daily lives.
The phrase "pregnancy is not a disease" is often echoed in clinics, but the medical reality is far more complex. "During pregnancy, a woman’s body undergoes numerous changes to support two lives," explains Dr. Noa Martonovich, a physician in the orthopedic department at Hillel Yaffe Medical Center. "Blood volume increases, as does cardiac output. Orthopedically, several processes occur. For instance, the body releases a hormone called relaxin, which helps loosen tissues and prepare the pelvic structure to expand for childbirth, allowing the baby to pass through the birth canal.
"However, this change stretches a joint beneath the groin, known as the pubic symphysis. While this physiological process is normal, in many cases, the joint stretches beyond the normal range – more than one centimeter – which can lead to significant pelvic pain," adds Martonovich.
Martonovich has been researching pelvic pain in postpartum women for years. "As a medical student, I joined Dr. Ran Tien, a sports orthopedist from Sheba Medical Center, to conduct a decade-long study tracking women who experienced pelvic pain after childbirth," she explains. "I delved into the academic literature and found conflicting data about the prevalence of this issue.
"Pelvic Girdle Pain (PGP) encompasses a variety of pathologies in nearby structures, which often present clinically as the same issue. I liken it to irritable bowel syndrome – many people suffer from it, but it’s not a single condition. It’s a collection of orphan diseases or phenomena that lack a clear definition."
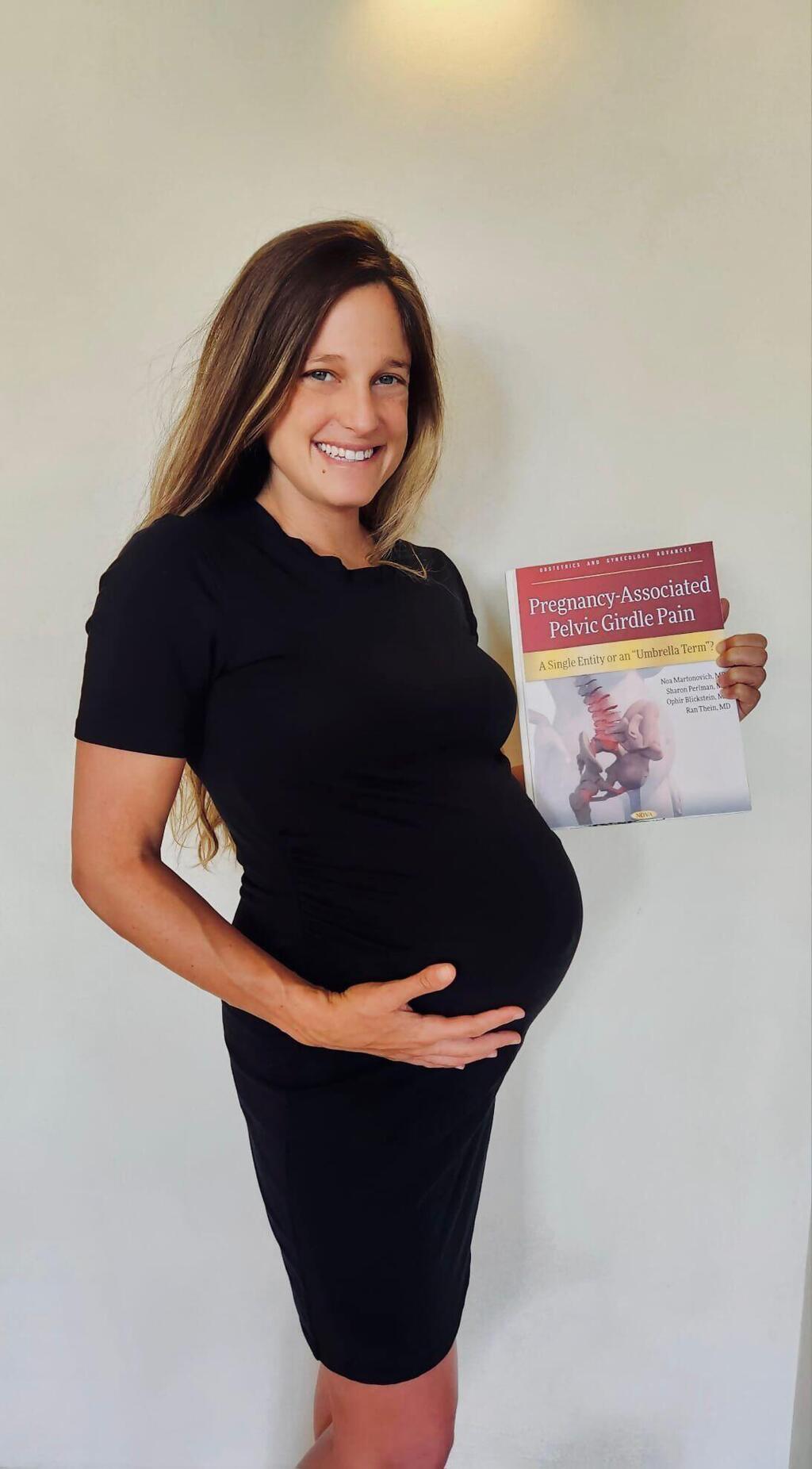
This subject is at the heart of a new book, "Pregnancy-Associated Pelvic Girdle Pain: A Single Entity or an Umbrella Term?", co-written by Dr. Martonovich, Dr. Tien, Professor Sharon Pearlman, and Dr. Ofir Blikstein, gynecologists from Rabin Medical Center. The book compiles historical research and studies on pregnancy- and postpartum-related pelvic, lower back and hip pain. It reveals that a significant number of women continue to suffer from pelvic pain even six months after childbirth. The professional literature reviewed in the book raises critical questions about the long-term consequences of these changes. Here are some key insights:
A significant gap in care
"There is a glaring gap between research and clinical practice," Martonovich emphasizes. "The lack of specialized expertise in musculoskeletal injuries related to obstetrics leaves many women stuck in a frustrating cycle of referrals between general practitioners, gynecologists and orthopedists. In my research, I’ve encountered women whose lives have been turned upside down by this pain – some haven’t returned to work, others struggle with daily activities, and some even require emotional support due to feelings of frustration and helplessness. Currently, there is no standardized treatment protocol. Some doctors refer patients for ultrasounds, which often provide only partial diagnoses, if any, while others recommend general physiotherapy without a specific framework."
Economic and social impact
Chronic pelvic pain after childbirth has significant economic and social implications. A study conducted at Sheba Medical Center by Martonovich and Tien found that 89% of women suffering from this pain did not return to their previous jobs, compared to 27% of the general population.
Over the long term, a decade after giving birth, many of these women still experienced persistent pain. Nine percent had not returned to work at all and remained unemployed, compared to 8% in the general population. Another noteworthy finding revealed that half of the women in the study had not reached the average family size in Israel, potentially indicating an avoidance of additional pregnancies due to fears of recurring or worsening pain.
Toward personalized medicine
"The next challenge is developing specific treatment protocols based on precise diagnoses," concludes Martonovich. She advocates for establishing a dedicated subspecialty in orthopedic care focused on musculoskeletal issues related to pregnancy and childbirth, a step that could bridge the gap between academic research and clinical treatment. However, she acknowledges that systemic change will take time.
Get the Ynetnews app on your smartphone: Google Play: https://bit.ly/4eJ37pE | Apple App Store: https://bit.ly/3ZL7iNv
"This is a global issue that requires systemic attention. Growing awareness is a first step, but comprehensive reform is needed in how the healthcare system addresses chronic pelvic pain in postpartum women. Steps that could help include conducting MRI scans for accurate diagnoses and establishing unique physiotherapy protocols tailored to each pathology."
First published: 10:57, 12.05.24