Bar-Ilan University has developed a new technology that assists the body’s immune system to fight cancer cells.
With research that began in 2016 Prof. Mira Barda-Saad and her team have made a “scientific breakthrough” in the fight against cancer, she told The Media Line.
The research published in the journal EMBO Molecular Medicine exposed for the first time the use of nanoparticles to remove obstructions that the tumor’s environment creates, which hinders the normal function of natural killer (NK) cells.
Barda-Saad says that “natural killer cells are lymphocytes that form the first line of immune defense against viral infections, tumor growth, and metastatic spread.”
Cancer researchers have identified for some time that NK-cells demonstrate a huge potential to treat cancer through immunotherapy as the cells produce a potent immune response in the vicinity of the tumor, resulting in a swift and direct killing of cancer cells in a tumor microenvironment (TME).
However, researchers have previously identified a challenge for the application of killer cells in immunotherapy, as the TME affects killer cells by evading or suppressing their activity resulting in cancer cells proliferating in tissues, an outcome which is detrimental to the bodies’ functioning capacities.
Barda-Saad and her research team at Bar-Ilan University have overcome this challenge by developing a mechanism to integrate lipid-based nanoparticles into the NK-cells. The harnessing of KC-cells with nanotechnology “dramatically enhanced the natural killer cells anti-tumor activity,” Barda-Saad said.
The nanocarriers are coated with antibodies that specifically recognize activated natural killer cells, which then target cancer cells, resulting in the reduction of the tumor size.
This is a significant development in the medical field as lipid-based particle nanotechnology used for temporarily silencing gene expression could not only be used to treat cancer, but also be used for other diseases.
Barda-Saad said that “by taking an anti-viral rather than an anti-tumor approach, it has opened the door for other uses,” including fighting viral infections and other pathological conditions. She added that this approach “is very powerful” in its possibilities for medical treatments.
As is the common practice applied to any new medical research, this strategy will undergo pre-clinical and clinical safety testing, a process that could take years. But Barda-Saad already has a goal in mind for these particles to be orally administered.
Prof. Deborah T. Blumenthal, director of the Neuro-oncology Service, Oncology Institute at the Tel Aviv Sourasky Medical Center-Ichilov, explained to The Media Line that creating nanoparticles in a form for oral administration “makes it user friendly because it’s easier for the patients, people who live further away wouldn’t have to spend their time coming into the hospital or the daycare center, they could then take it orally. It would be a huge bonus for them.”
3 View gallery
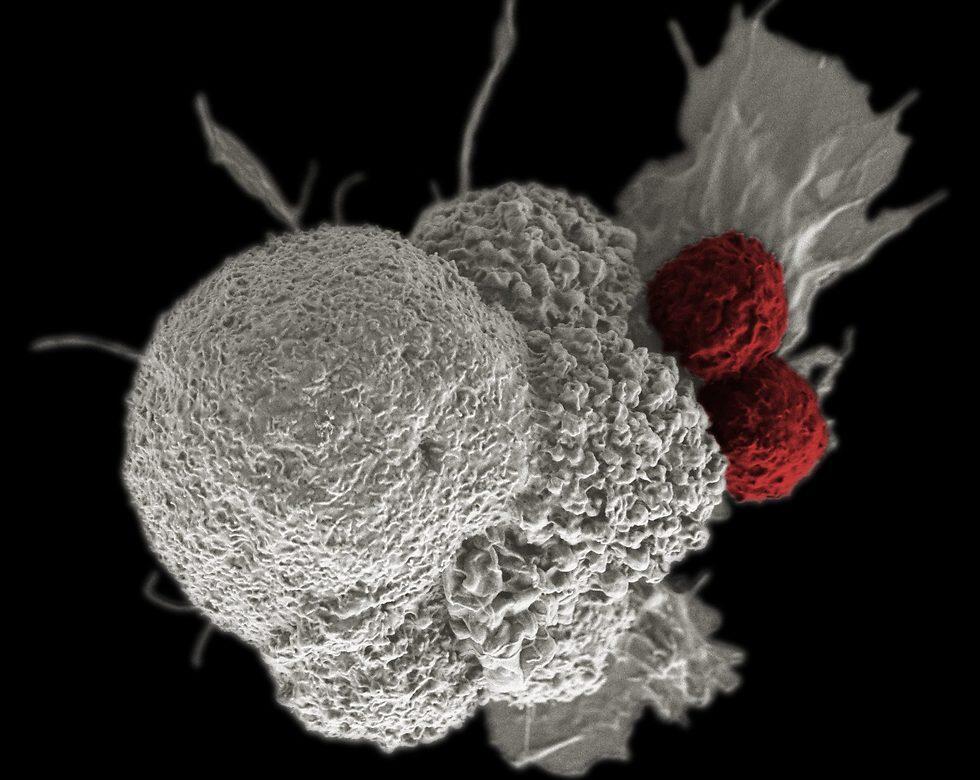
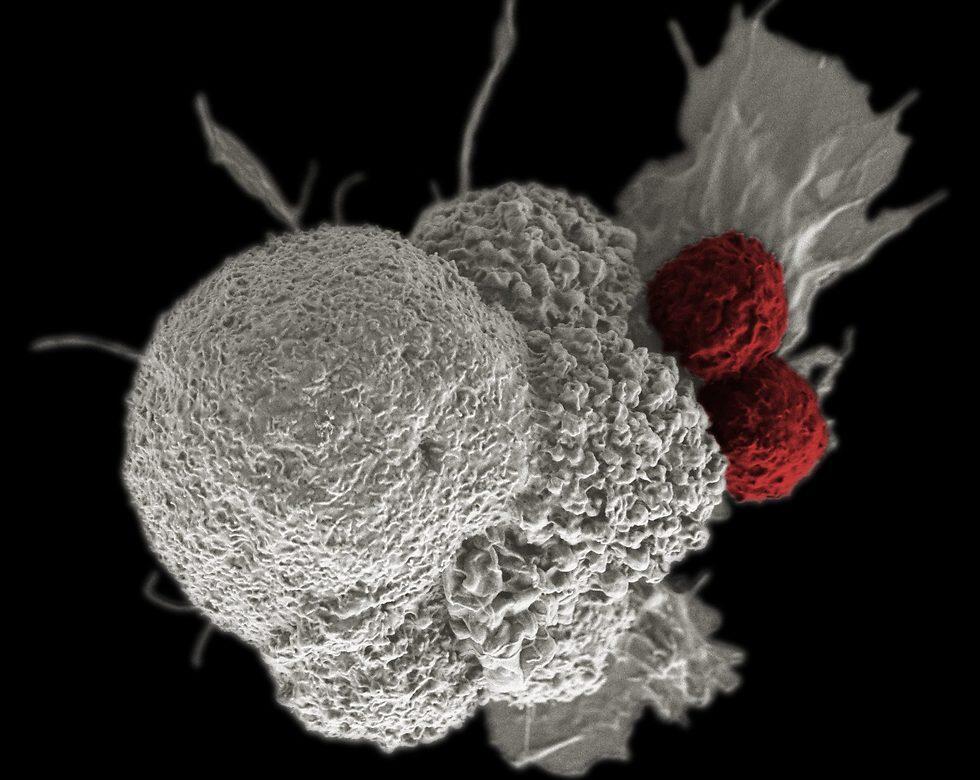
Cancerous tumor attacked by two T cells
(Photo: Rita Elena Serda, Duncan Comprehensive Cancer Center at Baylor College of Medicine, Nationa)
Not only would oral administration be beneficial to patients, but the precise, targeted method would allow for patients to opt for this treatment over preexisting treatments of chemotherapy or radiation therapy which are not ultra-selective and often have adverse side effects on patients.
Blumenthal said that “it’s a very intriguing and exciting concept,” specifically for the treatment of brain cancers. She said that these nanoparticles would bypass previous challenges over molecule size, which often meant biological treatments were unable to target the brain; however, a nanoparticle carrier would successfully target the brain and be able to target cancer cells found there.
With the World Health Organization declaring cancer as a leading cause of death in February, Barda-Saad sees this nanotechnology as a sign of a future of immunotherapeutic drugs to enhance the immune response against pathogens that cause illness. “I firmly believe that by combining it with the right molecules detected in our laboratory we will be able to harness it in the fight against cancer,” she said.