Blood, the liquid that flows through a branched network of vessels in our body, is essential for sustaining life. The blood supplies our organs with a wide variety of substances that are necessary for the proper functioning of our physiological systems, such as oxygen, nutrients and healing substances for our cells, while eliminating waste products such as carbon dioxide and unwanted substances such as pathogens.
The blood flows in our body in a continuous cycle, which is powered by the heart muscle. When this muscle contracts, blood is propelled into the aorta at the highest pressure found in the vascular system, and this pressure enables the blood to flow throughout the entire body, from the tissues nearest to the heart to those farthest away from it, nourishing the tissues and collecting their metabolic waste products.
The volume of blood in an individual’s body depends on their body’s size and weight. For instance, a healthy adult man weighing 70 kilograms typically has about five to six liters of blood. The temperature of the blood, 38 degrees Celsius, is on average one degree higher than the general body temperature, thus contributing to the regulation of the body's thermal balance.
Blood comprises mainly two types of cells: red blood cells, which transport oxygen, and white blood cells, which defend against infection. Additionally, blood contains essential materials and nutrients, including iron, calcium, glucose, and various minerals.
Thanks to the blood’s circulation through nearly all bodily tissues, it serves as a central hub for information and for monitoring the body’s state. The information stored in the blood can be extracted by simple blood tests, providing real-time and accurate insights into our health status and guiding appropriate treatment decisions when necessary.
5 View gallery


One of the treatments for blood component deficiency is blood transfusion: transferring blood or some of its specific fractions from a donor to a recipient. A woman donating blood
(Photo: Nastyaofly, Shutterstock)
Threefold essence: The layers of human blood
The color of the blood that cycles through a healthy body is a dark and uniform shade of red, but if we store the blood in a glass tube and wait for a day, or use a faster separation process, such as a centrifuge, we will see that the stored blood separates into three distinct layers that differ from each other in color and thickness.
The topmost layer is plasma, a yellowish fluid composed primarily of water and contains also proteins, sugars, minerals, gasses, and other substances. The plasma mainly serves as a liquid medium that facilitates the movement of substances throughout the blood vessels.Below the plasma lies a thin pink layer comprising blood platelets and white blood cells. Platelets play a critical role in blood clotting, preventing excessive bleeding, while white blood cells are key components of the immune system, protecting the body against infections. The bottom layer, bearing a dark red color, contains the heaviest blood cells, the red blood cells, which are pivotal in transporting oxygen from the lungs to other body tissues, to enable the process of cellular respiration.
Deficiencies in blood components may impair the functioning of body systems and lead to disease. One of the methods for treating such deficiency is by blood transfusion: transferring blood, or specific blood components, from a donor to a recipient.
In most cases, donated blood is separated into its fractions, red blood cells, plasma and platelets - allowing targeted transfusions tailored to the patient's requirements and ensuring optimal storage conditions for each fraction. For instance, anemia, which is caused by red blood cell deficiency and manifested in shortness of breath, fatigue, weakness, and headaches, can be effectively treated by transfusion of red blood cells.
5 View gallery
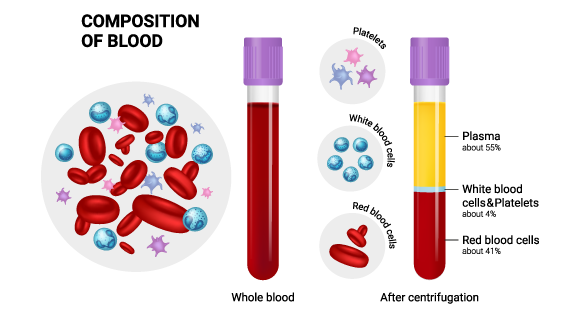
Fresh blood in a uniform red color (right) and blood separated into layers (left)
(Photo: LDarin, Shutterstock)
A bloody history
Blood transfusion is one of the most commonplace medical procedures in hospitals today. It is a life-saving intervention and is currently safe, though this was not always the case. The journey from the discovery of this technique as a method of saving lives to its safety and efficacy was fraught with challenges, claiming numerous lives and spanning many years of experimentation and discovery.
The first successful blood transfusion was performed in England in 1665, when physician Richard Lower transfused blood between two dogs. This blood transfusion laid the foundation for subsequent experiments in human blood transfusion. The initial attempts to perform a blood transfusion in humans used animal blood, such as sheep, and only later were trials conducted with human donor blood. Unfortunately, the blood transfusions caused severe immune responses in the recipients, which also resulted in death, and led to a temporary ban on further experimentation with blood transfusions.
Nearly a century and a half later, in 1818, obstetrician James Blundell documented the first successful human blood transfusion - a donation from a man that saved his wife's life who had lost a lot of blood in childbirth. Despite some sporadic successful blood transfusions, the enduring legacy of failed transfusions highlighted the need for a deeper understanding of the mechanism that enables a successful blood transfusion.
In 1900, a pivotal breakthrough occurred with the discovery of blood types by Karl Landsteiner, an Austrian physician of Jewish heritage. He was quoted saying that “The discovery of blood groups is one of the greatest scientific contributions to medicine”.
Indeed, this discovery paved the way to safe blood donations and today, a single blood donation can save the lives of three people. To honor Landsteiner’s legacy, his birthday, June 14th is celebrated as World Blood Donor Day, aimed at raising awareness of the critical importance of blood donations in saving lives.
Another significant milestone occurred in 1914, with the development of the technology for preserving blood donations. Prior to this advancement, donations had to be performed directly, necessitating the donor and recipient to be in close proximity throughout the procedure.
5 View gallery
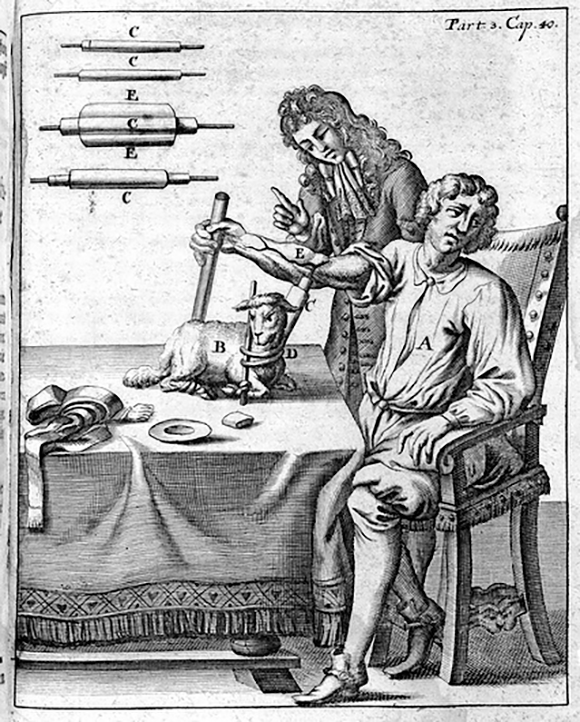
In the early attempts to perform blood transfusion in humans, Lower used animal blood. An illustration from 1692 describing blood transfusion between a lamb and a human
(Illustration: Wellcome Images / Science Photo Library)
The secret recipe for blood typing
Understanding blood groups and their importance in ensuring safe blood donation requires knowledge of red blood cells (RBCs) and antibodies. RBCs are mainly responsible for transporting oxygen to tissues throughout the body. Antibodies, which form an integral part of the immune system, and responsible for detecting and eliminating foreign and harmful elements that enter the bloodstream. Together, these components play a crucial role in determining compatibility for blood transfusions, ensuring that donated blood does not cause adverse reactions when introduced into another person's body.
In a healthy human body, there are RBCs of a specific blood group - and antibodies that do not recognize these RBCs as a foreign entity, but as a component that belongs to the body, thus avoiding harming them. However, if RBCs from a different blood group are introduced into a person's bloodstream, these are likely to be identified by antibodies as foreign, triggering a potentially fatal immune response known as hemolysis, in which the RBCs are destroyed. For decades, this severe immune reaction posed a risk of death in blood transfusions, until its mechanism was elucidated.And what is this mechanism?
The four blood groups: A, B, AB, and O, are determined by the presence or absence of specific antigens, or more accurately, by the specific composition of sugars present on the RBC membrane. RBCs of blood type A express A antigens on their surface. Those of blood type B express B antigens. RBCs with blood type AB express both A and B antigens and RBCs of blood type O lack these A and B antigens entirely.
In every blood type, in the blood’s plasma, there are antibodies for the antigen that is not present on the red blood cells of the same blood type. Type A blood carries type B antigens, type B blood carries type A antigens, type O blood carries both type A and type B antigens and type AB blood carries no antigens against red blood cells. Thus, if you accidentally treat a person who has type B blood with type A blood, the antibodies in his blood will identify the donated blood cells as invaders and attack them.
What about the addition of the plus or minus sign accompanying the blood type? Blood type determination involves not only the sugars but also the presence of the Rh protein on the surface of red blood cells. When the Rh protein is present, the blood is classified as positive (+), and when the protein is absent, the blood is classified as negative (-).
Once the blood type is identified and after verification of the presence or absence of antibodies for the Rh protein in the blood, blood donation can be conducted safely and appropriately, ensuring that recipients receive compatible blood types to avoid adverse immune reactions.
5 View gallery
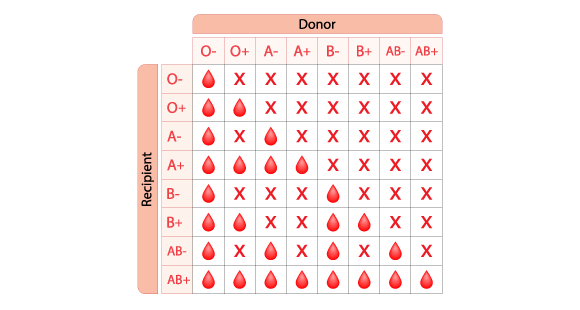
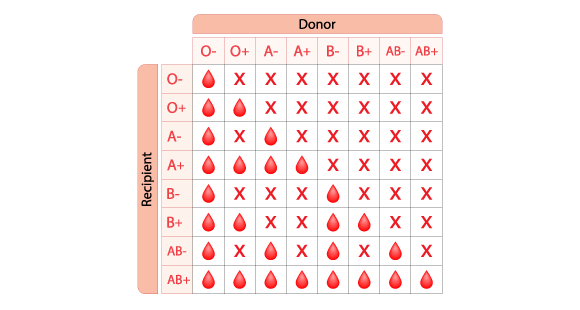
A table for matching the donor’s blood type with that of the recipient. For example, a person whose blood type is O minus can donate to everyone
(Photo: Ph-HY, Shutterstock)
The most prestigious blood type
In medical emergencies when blood transfusion is required urgently due to severe injury and massive blood loss, it is often impossible to immediately determine the patient's blood type. In these cases, the blood type that can be used safely, without fear of an immune response, is O negative. The reason for this is that the surface of RBCs of this blood type contains no antigens that the immune system could identify, so that even if the recipient’s blood has type A or type B antibodies, the transfusion will not trigger an immune response.
Thanks to this property, individuals with blood type O negative are universal blood donors; their blood can be given to any person, regardless of their blood type. As a result, the most sought-after blood type for donation is O negative, though it is one of the rarest blood types, accounting for only about seven percent of the population.
Blood type AB positive is also in high demand and is found in only four percent of the population. Its uniqueness is not in its red blood cells, as we have seen so far, but in its plasma. It contains no antibodies that might trigger an immune response against red blood cells, and therefore it can be used as a universal plasma donor, regardless of the recipient’s blood type. People with blood type AB positive not only have rare plasma that can save lives; since their blood lacks the relevant antibodies, they are also the only ones who can receive blood donations of any type, without fear of an immune response.
5 View gallery
People with blood type AB positive have no antibodies that could trigger an immune response against blood cells, and therefore they can receive blood donations of any type. The four main blood groups
(Photo: FOTOGRIN, Shutterstock)
How to donate safely
Blood is a complex liquid that cannot yet be produced in a laboratory, and therefore there is no alternative to blood donations. Blood donation is a simple, quick and life-saving procedure, but it is essential to proceed with caution and care to protect the health of both the donor and the recipient.
First, the donor must fill out a health questionnaire to determine if their blood could pose a risk to the recipient. If a person wishing to donate blood has diseases such as viral hepatitis, leukemia, lymphoma, tuberculosis, or brucellosis, their blood would be dangerous for the recipient, and thus they would not be allowed to donate blood.
Additionally, it is important to assess whether the donor is medically fit to donate blood - if they can afford to lose blood without harming their health. To protect the donor from medical complications, blood donation is restricted in conditions such as pregnancy, a previous blood donation within the last three months, hypertension or hypotension, severe reactions to previous donations, anemia, a tendency for bleeding and active asthma.
The volume of one blood donation is about half a liter, and additionally, a few blood samples are taken to rule out diseases such as viral hepatitis and HIV. The blood is separated into its fractions, which have different shelf lives: red blood cells are viable for forty days, platelets last for about five days, while plasma lasts about a year.
Blood is one of the most important and complex tissues in the human body. It currently has no artificial substitutes, by adhering to simple and secure procedures, blood can be safely preserved and transfused, effectively saving lives in the process.

