Getting your Trinity Audio player ready...
A statement from a Melbourne-based research institute in Australia about a potential breakthrough in treating pediatric heart failure using stem cells captured the imagination of researchers and doctors worldwide. However, Israeli experts noted that the "Holy Grail" of this complex field hadn’t yet been found and practical application remained a distant goal.
Researchers at the Murdoch Children’s Research Institute (MCRI) in Melbourne developed an innovative approach by creating "beating heart models" under laboratory conditions. The process began by extracting white blood cells from humans.
Using specialized materials, the researchers transformed these white blood cells into stem cells. The stem cells were then differentiated into heart muscle cells, effectively constructing an active heart model in the lab.
Prof. Kobi George, head of Kaplan Medical Center’s cardiology unit, explained: "This process converts blood or skin cells from patients back to their basic state as stem cells, which are then differentiated into heart cells. These cells can potentially be rebuilt and implanted into the damaged heart to improve its function."
The innovative treatment targeted heart failure caused by congenital defects and damage from chemotherapy in children, especially from anthracycline drugs which can lead to heart failure in up to 15% of cases.
Prof. Ran Kornowski, head of Rabin Medical Center’s cardiology unit, said that while the study appeared promising, it was important to acknowledge the complexity of the field, which still required extensive study and years of development. "This is a step in the right direction," he said, "but we're far from cracking the formula or finding a 'magic solution' for congenital heart diseases."
Heart failure in children can be deadly
"Heart failure predominantly occurs in adults, with coronary artery disease, including narrowing and blockages in heart vessels and repeated heart attacks as primary causes," Prof. George explained. "Key symptoms include shortness of breath and fluid accumulation in the lungs or other parts of the body."
He noted that heart failure was the leading cause of hospitalizations worldwide among those over 65, making it a focal point for medical research and development. Significant progress has been made in the area in recent years, with breakthroughs and new drug treatments demonstrating their effectiveness.
"This is a dynamic and active field where substantial efforts are invested to improve patients' quality of life," he added.
What about children?
"The story is entirely different in children," said Prof. George. "Most cases of heart failure result from genetic factors, such as mutations or defects in genes responsible for the heart muscle's proper function, particularly its ability to contract correctly. Mutations affecting these genes lead to heart failure at a very young age, as the heart struggles to meet the high demands of an infant's rapid and powerful cardiac activity.
“This manifests as fluid accumulation in the lungs, breathing difficulties, decreased blood oxygen levels and a significantly increased respiratory rate. In severe cases, infants may experience respiratory distress."
According to Prof. George, an estimated half a million infants and children worldwide suffer from heart failure. "Treatment for these infants is purely symptomatic as no current method directly addresses the root cause," he said.
"The primary goal is to alleviate symptoms, particularly by reducing fluid buildup in the lungs and body. This is achieved using various medications that enhance kidney function and promote urination, thereby removing excess fluid from the body. While this provides significant relief, it doesn’t resolve the underlying problem,” he added.
Once the infant's condition stabilizes, additional medications are introduced to reduce the load on the heart muscle by lowering blood pressure. "This treatment allows for relative improvement and better coping ability but doesn’t lead to complete recovery. Mortality rates among infants with heart failure remain very high," he added.
'Still far from widespread application'
Stem cell therapy and tissue engineering are at the forefront of medical innovation, offering the potential to transform the lives of children and adults with heart failure. This field is based on a simple yet powerful principle: adding healthy muscle tissue to the heart could enhance its function and contraction capability.
Prof. Kornowski recounted leading an international study in 2002 at Rabin Medical Center, where stem cells were implanted in adult patients with severe heart conditions. "The study generated significant hope, especially given that we implanted autologous cells taken from patients’ bone marrow and reintroduced them into their hearts.
“The initial results were highly promising, but the method failed to become a comprehensive breakthrough or a commercial product. Since then, stem cell research has experienced ups and downs, remaining an active field of study but still far from widespread application."
Get the Ynetnews app on your smartphone: Google Play: https://bit.ly/4eJ37pE | Apple App Store: https://bit.ly/3ZL7iNv
He stressed the increasing realization of the field’s complexity as research progressed. "It’s important to manage expectations when it comes to studies that promise a cure for congenital heart diseases using stem cells.
“Congenital heart diseases encompass a broad and diverse range of medical issues and it’s unrealistic to expect this technology to address all of them. Some cardiac defects are too complex for stem cells to provide a complete solution."
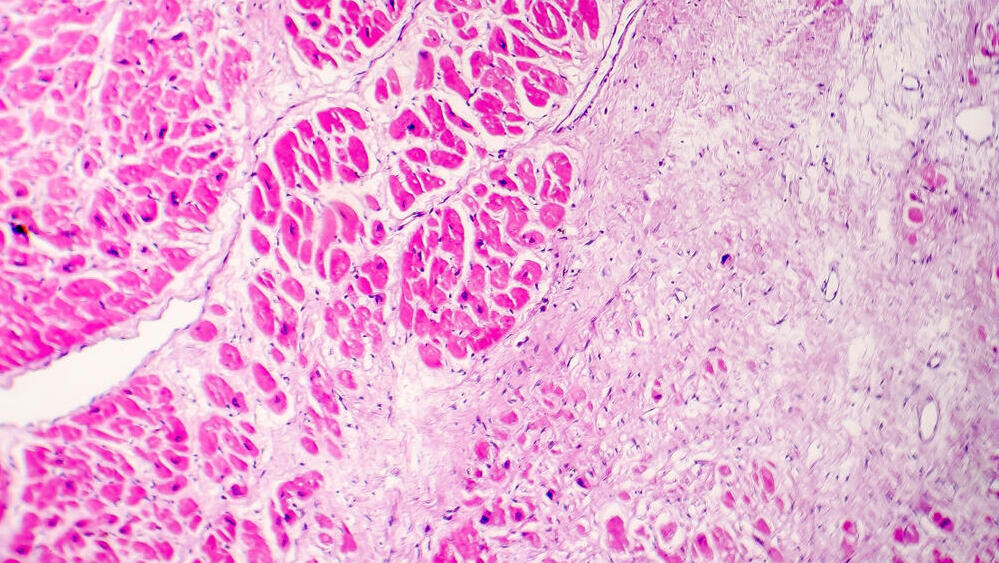
Prof. George noted that numerous attempts to implant stem cells into the heart had been made over the past 25 years using various methods. A key approach involved using bone marrow-derived cells — "primitive" cells with the potential to differentiate into various tissue types.
"These cells were injected directly into the heart muscle or the arteries leading to the heart, with the hope that they’d reach the damaged area and regenerate the heart muscle. These trials focused primarily on adults, but unfortunately, the results didn’t meet expectations over the years."
He mentioned a revolutionary discovery a few years ago that earned researchers Shinya Yamanaka and John Gurdon the Nobel Prize. The discovery demonstrated the ability to revert ordinary cells, such as skin or blood cells, into stem cells through a sophisticated process.
"This capability sounds almost like science fiction: by introducing a specific set of genes, ordinary cells, called somatic cells, can be 'rewound' into their undifferentiated stem cell state," Prof. George explained. "Stem cells have immense potential as they can differentiate into any tissue type in the body — skin, hair, brain, kidneys, heart and more.”
“They represent the initial stage of all bodily tissues. As the cells mature, they become more specialized and assigned to specific organs. The new discovery allows already specialized cells to be returned to their original state, enabling them to 'grow' into any required tissue. Think of it as a tree trunk, from which leaves emerge,” he explained.
What’s the issue with this Nobel Prize-winning technique?
Prof. George highlighted that using somatic cells to produce stem cells held tremendous medical potential but also posed significant risks, including the potential for cancerous processes due to gene insertion into DNA during the procedure.
Despite successfully producing functional heart muscle in the lab, Prof. George stressed that the heart is an exceptionally complex organ, with a unique nervous system, a natural pacemaker and other critical components.
Creating a fully functioning heart model remains a significant challenge. Nevertheless, the ultimate goal in modern medicine is to engineer lab-developed cells, convert them into specialized stem cells and reimplant them into damaged hearts to restore functionality.
To date, trials have been conducted on animals such as mice, sheep and pigs, demonstrating success. The research is now expected to progress to clinical trials on humans. The technology could potentially benefit patients of all ages, though current lab trials are focused on children.
Researchers believe stem cells will integrate more effectively in children over time and have an optimal impact on heart function.
"The novelty lies in the ability to reprogram a person’s white blood cells into stem cells using special materials, which were then used to build beating heart models," Prof. George concluded.
A new hope
Prof. Kornowski added that if these studies succeed, the breakthrough could be transformative. "We could repair non-functioning heart regions, providing at least a partial alternative to heart transplants or artificial hearts. This is the great hope driving the field. However, transitioning from animal-based technologies to human applications is an enormous challenge.
"Having worked in both lab research and patient care, I’m acutely aware of the depth and complexity of these challenges. A combination of cell implantation, genetic treatments and other methods might yield better results than any single approach — but much more research is needed to prove this," he concluded.