The brain is the central organ responsible for our thoughts and emotions, as well as for the feedback that enables us to perform activities such as walking, singing, and dancing.
Other stories:
In addition to these well-known functions, the brain is also involved in controlling other systems we may not typically associate with it. For instance, signals from the brain can influence our breathing rate, blood pressure, urine production, and the body's response to disease.
6 View gallery
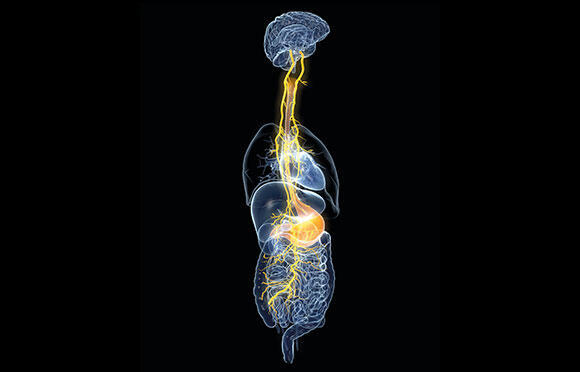
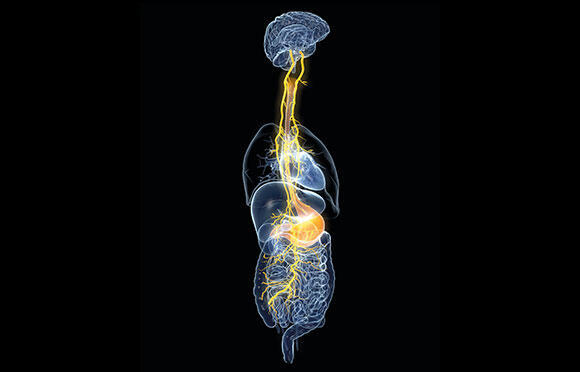
When the brain signals to the enteric nervous system, it does so through a special nerve called the vagus nerve
(Photo: Axel_Koc, Shutterstock)
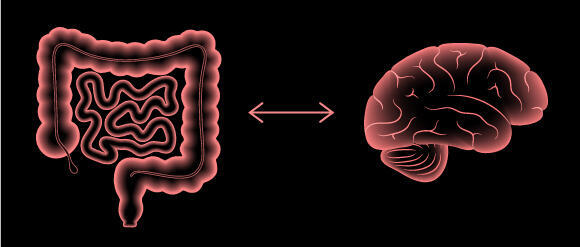
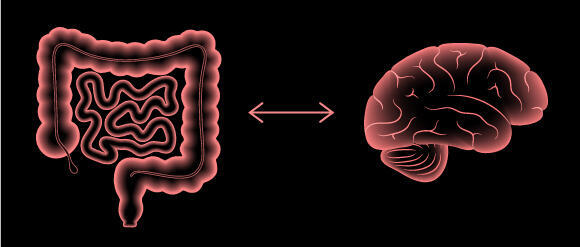
The brain also communicates with the digestive system, influencing its activity and the amount of blood allocated for digestive processes. In recent years, a fascinating sequence of discoveries has taught us that the relationship between the gut and the brain is bidirectional: not only does the brain affect the digestive system, but the digestive system also has significant effects on the brain, impacting our sensations, and mental state.
The intricate communication between the gut and the brain is known as the "gut-brain axis". It involves the nervous system, the hormonal system, as well as the activity of bacteria residing in the gut.
In this article, we will present some of the research exploring the intricate relationships and mutual influences between the brain and the gut, as well as on the role of the populations of gut bacteria involved in this dynamic interaction.
Butterflies in the stomach
The nervous system connects the brain to all other organs in our body. This system comprises an intricate network of nerve cells that transmit signals to each other in the form of fast electrical pulses. Given the vital role that the digestive system plays in our daily functioning, it is not surprising that the nervous system also interacts with it.
The enteric nervous system consists of a network of nerve cells that envelope the digestive organs, extending from the esophagus to the anus. This extensive nervous system contains approximately 500 million nerve cells, and operates largely independently, functioning without frequent signals from the brain. Its high level of autonomy has earned it the nickname the "second brain".
Communication from the brain to the enteric nervous system occurs via a special nerve, the vagus nerve. The vagus nerve emerges from the brainstem - a primitive part of the brain that controls basic functions such as breathing, blood pressure regulation, and eating processes such as chewing, swallowing, and appetite.
The vagus nerve, which originates from it and traverses the chest and abdominal cavity, is one of the longest nerves in the human body. It not only interacts with the digestive system, but also innervates other vital organs, such as the heart and lungs.
The vagus nerve enables fast communication between the brain and the gut, and through it, the brain can direct changes in the activity of the intestinal muscles, stomach acid release, and the contraction of the muscles of the bladder.
However, this communication is not unidirectional. The vagus nerve not only transmits signals from the brain to various organs but also receives signals from these organs about their condition to relay back to the brain. For example, it detects substances released from the cell layer lining the intestine, enabling it to signal the amount of food present in the digestive system and allowing the brain to adjust the hunger sensations accordingly.
The digestive process also triggers the secretion of various hormones, which the vagus nerve detects and signals to the brain to reduce sensations of hunger. Conversely, when there is no food in the digestive system, other hormones are released, which the vagus nerve identifies and signals to the brain to increase hunger sensations.
The army that marches on our stomachs
A significant factor that has a tremendous impact on the activity of the digestive system is the microbiome. This term refers to the symbiotic community of microorganisms, including bacteria, fungi, and viruses that live within us.
6 View gallery
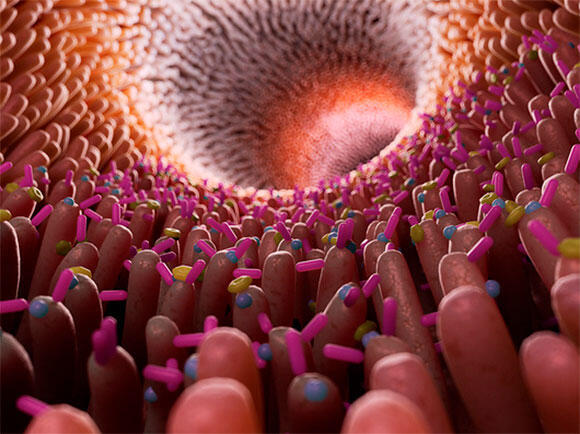
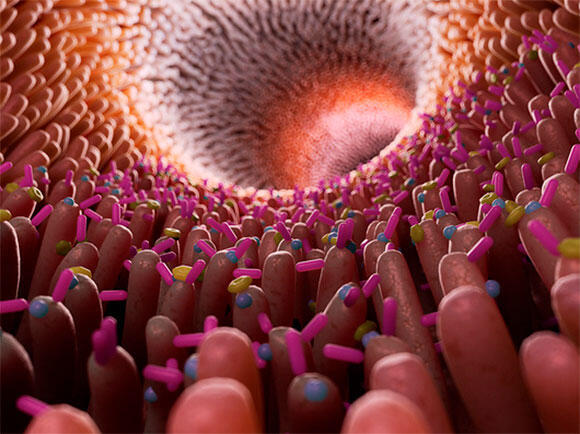
The microbiome is a significant factor that has a tremendous impact on the functioning of the digestive system
(Illustration: Sebastian Kaulitzki / Science Photo Library)
While we are used to thinking of bacteria as foreign and harmful factors that sneak into our bodies and need to be eliminated as quickly as possible, this is not always the case. In fact, our body is home to billions of bacteria that not only do not harm us, but are in fact beneficial.
These symbiotic relationships are beneficial to both parties involved: the bacteria inhabit an environment suitable for their survival and rich in nutrients, while their host benefits from the bacteria’s ability to break down and metabolize substances.
Moreover, these non-pathogenic bacteria occupy the appropriate niches within our body, preventing the growth and establishment of pathogenic bacterial populations.
If we specifically examine gut bacteria, we find that they help us digest the dietary fibers in our food and extract nutrients from them. It is not surprising that gut microbiota also has a significant impact on the likelihood of developing obesity.
In a study that examined the link between obesity and gut bacteria, researchers took samples of gut bacteria from identical twin couples, one of whom was thin and the other overweight.
The bacteria were then implanted in the intestines of mice, and after a short time, the mice that received the bacteria from the overweight twin gained weight, while the mice that received the gut bacteria from the thin twin maintained a normal weight. It is clear, therefore, that these bacteria have a significant impact on food consumption and metabolism in the body.
The gut-brain axis
The influence of gut bacteria on mental health, anxiety, social behavior, and even potential links to schizophrenia
The influence of gut bacteria extends beyond the digestion and breakdown of food. As research progresses, it is becoming clear that gut bacterial populations play a significant role in how the gut affects the brain.
A study conducted in the 1990s demonstrated that certain bacteria in the digestive system of mice could alter the animals’ behavior and cause symptoms of stress and anxiety. This study was the first to demonstrate that the influence of gut bacteria on the brain and animal behavior is independent of the activation of the immune system.
Subsequently, another study showed that gut bacteria can alter the body’s stress response by affecting brain regions such as the hippocampus, amygdala, and prefrontal cortex. These three regions are responsible for the hormonal "fight or flight" response, in which hormones such as cortisol and adrenaline are released into the bloodstream to prepare the body to handle a threatening situation.
For example, a recent study found that when gut bacteria from humans who had experienced trauma and suffered from anxiety were transplanted into the intestines of mice, the mice started to exhibit anxious behavior. This suggests that changes in the composition of gut bacteria can directly affect animal behavior.
In the same study, researchers also examined the gut bacteria composition of individuals experiencing prolonged stress and found that it was different and less diverse than that of healthy individuals. Moreover, gut bacteria can even produce neurotransmitters, such as serotonin and dopamine, and thus may potentially directly influence our mood.
It is important to emphasize that these studies were conducted on mice, a model organism with limited predictive value for human responses. While the findings suggest similar effects might occur in humans, more comprehensive research is required to confirm these connections.
Can opposing emotions, such as calm and tranquility, be tied to the composition of gut bacteria? Research suggests they can. For instance, one study examined the gut bacteria of Buddhist monks who practice deep meditation and identified bacterial populations associated with low levels of stress and depression in their guts. These bacterial populations were not found in the guts of nearby residents who do not practice meditation.
6 View gallery
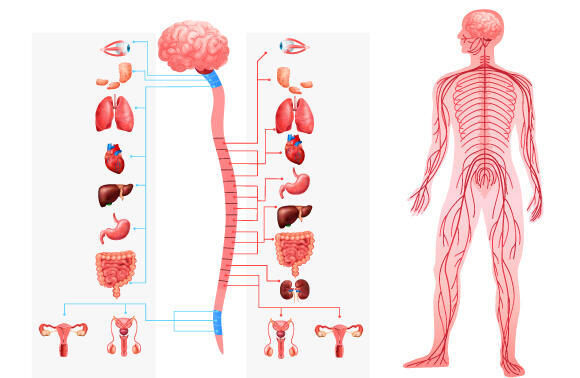
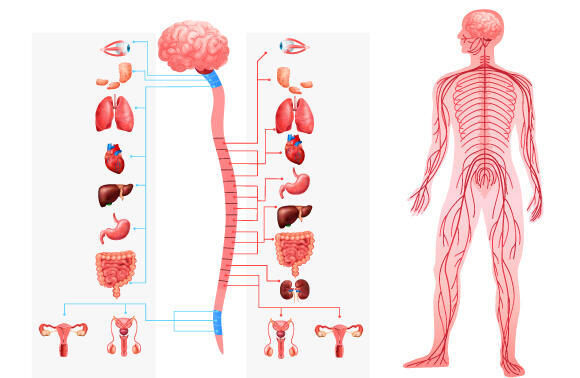
The nervous system, including the vagus nerve, connects the brain to the rest of the organs in our body
(Illustration: Macrovector, Shutterstock)
Another study found a link between a diverse population of gut bacteria and the ability to build strong social relationships. Conversely, individuals with autism spectrum disorder, who have difficulty with social understanding, and individuals who suffer from anxiety and stress, had a narrower range of gut bacteria.
It is important to note that in such studies, it is difficult to distinguish between different characteristics of the subjects, such as their mental state and their diet. For example, autism is often associated with difficulties in maintaining a balanced and diverse diet, and it is not easy to isolate and distinguish the influences and impacts of the various factors involved - neurological diversity, diet, and gut bacteria.
In this study, using statistical analysis, researchers were able to conclude that a relationship exists between sociality and gut bacteria diversity that cannot be solely explained by diet.
Gut microorganisms may indirectly affect brain function if they trigger chronic inflammation, leading to an overactive immune system. Studies have found a link between neurodegenerative diseases such as Alzheimer's and Multiple Sclerosis, and certain populations of gut bacteria.
Some of this influence seems to be related to the inflammatory response to these bacteria. Chronic inflammation can damage the blood-brain barrier, which, in its normal state, prevents harmful substances from the bloodstream from entering the brain.
Individuals with neurodegenerative diseases often have a more permeable blood-brain barrier, which allows a higher-than-normal amount of substances to cross from the bloodstream into the brain.
Additionally, anecdotal evidence suggests a connection between inflammatory responses in the gut and mental disorders, such as schizophrenia. The biological mechanisms underlying mental disorders are highly complex, and further research is necessary to understand the interplay between gut bacteria, the immune system, and the brain in this context.
Cultivating the right bacteria
We accumulate bacteria in our bodies throughout our lives, particularly during periods of growth and development. Breast milk that we consume as infants and the food we eat as children are important sources of beneficial bacteria.
6 View gallery
Gut microorganisms may indirectly influence brain function
(Illustration: Pikovit, Shutterstock)
Different bacteria favor different foods, indicating that the composition of our diet can influence our gut microbiota population and, consequently, our mental state. For instance, increased sugar consumption has been linked to anxiety symptoms, while tea consumption appears to somewhat reduce the likelihood of depression.
Physical activity is another factor that influences our gut microbiota population. Although this topic still requires long-term research, evidence already indicates that early-life physical activity has a positive effect on gut microbiota population and metabolic health.
The use of antibiotics to help us fight harmful, disease-causing bacteria that enter our bodies, can also alter the gut microbiota population. Furthermore, the gut microbiota population is also affected by aging.
The interconnected body
We often perceive the brain as the organ controlling and coordinating the body's systems. However, it’s important to remember that our body's functioning relies on interconnected systems that mutually influence each other. The brain and nervous system are no exception, with a reciprocal relationship existing between the digestive system and the nervous system, particularly the brain.
Gut bacteria play a central role in this reciprocal relationship. As our understanding of their impact on the brain deepens, we come closer to being able to potentially utilize changes in gut microbiota for therapeutic purposes.
In the not-too-distant future, we might be able to treat a variety of conditions and disorders by the simple means of transplanting gut microbiota. In the meantime, we must continue to investigate these fascinating mutual relationships and strive to optimize them by maintaining a healthy lifestyle.
Content distributed by the Davidson Institute of Science Education.



