Blood is life. At every moment, blood transfusions are saving lives in hospitals, emergency rooms, and disaster zones worldwide. Yet the global supply of blood depends entirely on human donors—a system vulnerable to disruptions from pandemics, wars, and natural disasters. With increasing demand and logistical challenges, a groundbreaking innovation is emerging from Israel to address the fragility of blood supply systems.
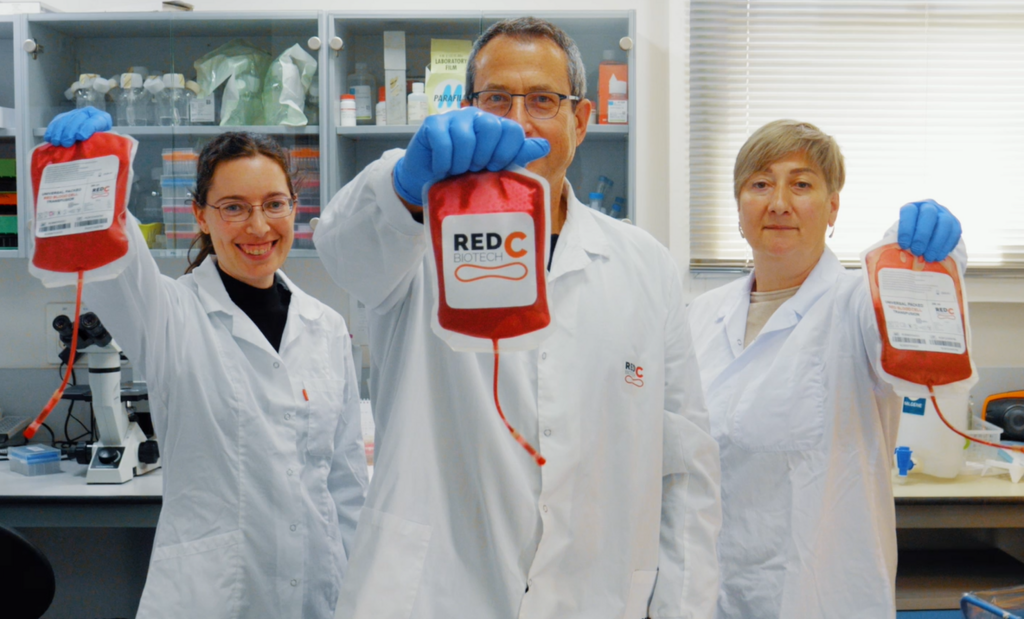
An Israeli startup, RedC Biotech, has developed a technology that could revolutionize blood supply by producing high-quality, safe, and cost-effective red blood cells (RBCs) on a mass scale using stem cell technology. The company aims to create universal RBCs that are compatible with any recipient without testing, free from contaminants or risky donor-derived residues. RedC Biotech’s ambitious vision is to address the global blood shortage crisis within the next five years.
“Red blood cells make up about half of the volume of our blood,” said Dr. Ari Gargir, founder of RedC Biotech. “While other components like plasma and platelets are critical, red blood cells are essential for carrying oxygen, making them vital for life-saving treatments. Our technology is focused on developing an industrial process to produce unlimited, universal red blood cells without the need for donors. The goal is to use them for life-saving transfusions and advanced therapies.”
Gargir explained that the need for RBC transfusions is constant and widespread. “Every hospital department uses red blood cell transfusions for patient care,” he said. “Most people associate blood transfusions with trauma victims—those injured in combat or accidents who need both fluid volume and oxygen-carrying capacity restored. Decades ago, patients received only saline infusions, and many died simply because their blood couldn’t carry oxygen.”
But trauma is only one scenario. Gargir highlighted other critical use cases, including surgeries and childbirth. “During major surgeries, patients lose significant blood, and postpartum hemorrhage is another leading cause of maternal deaths—around 200,000 women die annually due to blood loss during childbirth,” he said.
Chronic conditions also require consistent RBC transfusions. Patients with hereditary diseases like sickle cell anemia or thalassemia depend on regular blood transfusions, as do those with severe jaundice or kidney diseases. “Some patients need just a few units annually, but others require dozens—sometimes one or two units every week,” Gargir noted.
Cancer patients are another major group. “For those with leukemia or undergoing chemotherapy and radiation, their ability to produce red blood cells is often compromised. I recently spoke with someone battling leukemia who had received nearly 200 blood units since last August,” Gargir said.
The current blood donation system faces several limitations that RedC Biotech seeks to overcome. "Blood comes exclusively from human donors, but even the most altruistic donors can only donate every three months,” Gargir pointed out. “Over-donation can lead to anemia as their iron stores deplete.”
Get the Ynetnews app on your smartphone: Google Play: https://bit.ly/4eJ37pE | Apple App Store: https://bit.ly/3ZL7iNv
He also emphasized how external factors disrupt donations. “Holidays, extreme weather, wars, or pandemics can keep people from donating blood. Imagine thousands of rockets raining down during a war or a severe earthquake—people wouldn’t be able to leave shelters or reach donation centers. The system would collapse,” he said.
Another significant hurdle is the short shelf life of blood. “RBCs have a shelf life of about 32 days. This creates logistical challenges. Blood can be frozen, but that process requires anti-freeze agents that can damage the cells,” he explained.
Economic factors compound the problem. Gargir revealed that the cost of a single blood unit averages $200 globally but can reach $600 when factoring in testing, logistics, and other processing costs. “Think about a patient requiring ten units during surgery—that’s $6,000. In Israel, the costs are subsidized, but globally, this is a significant challenge,” he said.
Artificially manufactured human blood
For Gargir, the issue of blood supply is deeply personal. “Thirty years ago, as an undergrad, I had a paragliding accident that burst my lungs. I needed emergency surgery and received a blood transfusion mid-flight,” he recalled. “I distinctly remember asking the doctor, ‘Was this blood tested?’ It was the early days of the HIV epidemic. That experience made me realize how complex and fragile the blood supply chain is.”
RedC Biotech’s solution involves manufacturing RBCs from stem cells in a lab. “We use specialized stem cells,” Gargir explained. “Stem cells are remarkable—they can divide indefinitely and transform into any type of cell the body needs. By replicating the body’s natural processes, particularly in bone marrow, we guide these cells to develop into red blood cells.”
Gargir likened the process to cultivated meat technology. “It’s similar to growing lab-based meat, where stem cells or fibroblasts are turned into muscle, fat, and connective tissue. We do the same thing but produce red blood cells,” he said.
Currently, the company operates at a relatively small scale in its lab. The plan is to gradually scale up production over the coming years, progressing to preclinical trials, clinical trials, and eventually industrial-scale manufacturing. “Many labs have successfully produced RBCs, but scaling the process to make it cost-competitive with donated blood has been the challenge,” he noted.
Gargir acknowledged the enormous challenges ahead. “Our goal is to begin preclinical trials in two years, followed by clinical trials, and ultimately launch commercially,” he said. The company is crowdfunding through the PeopleBiz platform to support its efforts.
The long-term vision is ambitious. “We envision factories worldwide producing universal red blood cells under local regulations and selling directly to hospitals or blood organizations. Imagine having two or three factories in Africa, Asia, or the U.S., ensuring that every region has access to a reliable blood supply,” he said.
Gargir also highlighted two additional goals for the future. “One is developing a substitute for whole blood, which is critical for scenarios like battlefield injuries. The other is creating blood that can be dried and stored at room temperature, making it accessible to remote or underserved areas. The ultimate dream? Sending these blood supplies to space stations or on interplanetary missions, ensuring human safety far beyond Earth.”
While artificial blood may still sound like science fiction, RedC Biotech is determined to make it a reality. If successful, the technology could transform global healthcare, ensuring that life-saving blood is available to anyone, anywhere, at any time.